Research in the Zhang Lab
Epigenetic regulation of T cell allo-immunity and tumor-immunity
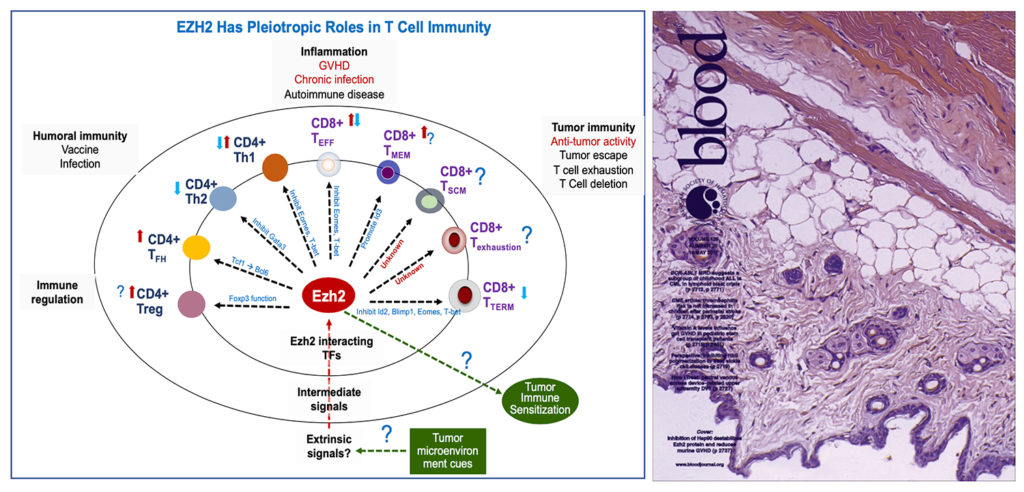
Dr. Zhang’s laboratory investigates epigenetic regulators that regulate effector T cell production and memory T cell formation in the context of allogeneic hematopoietic cell transplantation (allo-HCT) and tumor immunotherapy. T cells play critical roles in the adaptive immunity against infections and tumors. Upon antigenic activation, they can differentiate into effector cells to eliminate the immediate threat, while producing memory T cells that have longer lifespan and can rapidly produce effector cells upon antigenic rechallenge. Persistent effector T cells can cause the destruction of normal host tissues (such as graft-versus host disease and type 1 diabetes), whereas T cells with impaired memory potential are unable to clear chronic infections or tumors. Dr. Zhang and colleagues have identified that Ezh2, a chromatin-modifying enzyme that orchestrates multiple gene programs, is crucial for promoting effector T cell survival and persistence, preventing differentiation of antigen-experienced T cells into terminal effector cells, and regulating memory formation and recall response (Kato et al. BBMT 2010, He et al. Blood 2012, He et al. Blood 2013, Tong et al. J Immunol 2014, He et al Nat Communications 2017, and Ji et al. Nat Communications 2019). Dr. Zhang’s laboratory also discovered that Hsp90 is required to maintain Ezh2 protein stability in activated T cells. Pharmacological inhibition of Hsp90 destabilizes Ezh2 protein in activated T cells and reduces graft-versus-host disease. Targeting the Ezh2-Hsp90 complex may represent a novel and clinically relevant approach to modulate graft-versus-host disease. This discovery is a cover story in Blood (Huang et al. Blood 2017). Currently, Dr. Zhang’s lab investigates how Ezh2 in T cells converts environmental signals into intrinsic transcriptional programs to influence effector and memory T cells, and how Ezh2 inhibition causes cell death in antigen-driven T cells. The goal of these studies is to identify Ezh2-targeted molecular pathways for improving the efficacy of tumor immunotherapy and allo-HCT.
Alloimmunity, dendritic cells and epigenetic regulation
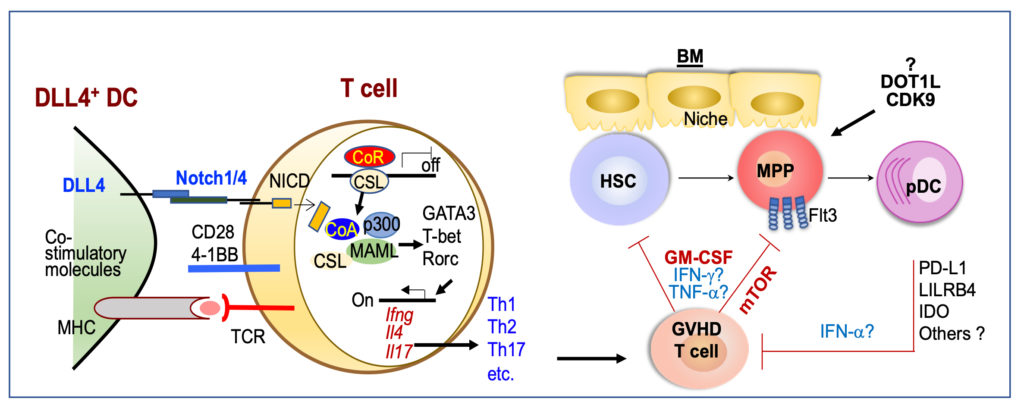
A second major focus in Dr. Zhang’s laboratory is studying the molecular mechanisms that mediate immunogenic activity and tolerogenic effects of dendritic cells (DCs). DCs are essential for initiating primary T cell immune responses and licensing effector T cells to eliminate tumors and induce graft-versus-host disease. Dr. Zhang and colleagues discovered that inflammatory stimuli induce DCs to produce high levels of DLL4, a Notch ligand that activates Notch signaling in T cells to instruct their differentiation into CD4 helpers (Th1, Th2 and Th17cells) and effector CD8 T cells (JI 2013, JI 2016, Blood 2016). Using these DLL4+DCs, the Zhang lab developed a clinically relevant strategy to program donor T cells that have potent anti-leukemia activity without mediating severe graft-versus-host disease in preclinical models (Blood 2016). Notably, DCs also play important roles in mediating tolerance of T cell responses against many types of antigens, such as self-antigens, tumor antigens and alloantigens. The Zhang lab revealed that plasmacytoid dendritic cells (pDCs), which specialize in production of type I IFNs and anti-viral immunity, play important roles in modulating antigen-driven T cell responses. Adoptive transfer of donor-derived pDCs inhibits graft-versus-host disease, preserves potent anti-leukemia activity, and improves reconstitution of immune cells (such as B cells) in leukemia mice undergoing allo-HCT (JCI 2021). Zhang and colleagues also discovered that inflammatory T cell responses deplete DC progenitors, causing donor pDC defects. In human patients, low pDC counts in the circulating blood are a valuable biomarker for predicting the occurrence of severe GVHD (JCI 2021, TCT 2021). Currently, the Zhang lab focuses on identifying which epigenetic regulator(s), such as DOT1L and CDK9, may play crucial roles in pDC generation and function, and whether inflammatory T cells may target these epigenetic regulators to induce pDC defects in allo-HCT patients. The goal is to establish pDC-based cellular therapy and pDC biomarkers to translate into patients.
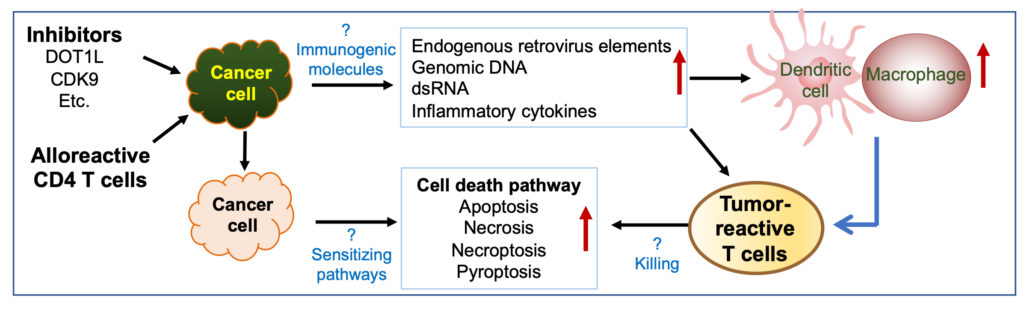
Targeting epigenetic regulators in tumors to sensitize cancer immunotherapy
The Zhang lab is interested in establishing novel approaches to reduce tumor resistance to cancer immunotherapy. Immune-based therapies have been transformative; however, they are only effective in a subset of cancer and patients. Tumor resistance to immunotherapy is likely multifactorial, involving lack of tumor-reactive T cell persistence and function, target antigen escape, and suppressive tumor microenvironment. Epigenetic dysregulation is a common feature of most cancers and may shape tumor immunity. Inhibition of CDK9, an epigenetic repressor and transcriptional elongation regulator, activates the expression of immune response genes, including antigen-presenting molecules and immune-checkpoint inhibitors (ICI), leading to partially restored ICI’s anti-tumor activity in mice with ovarian cancer (Zhang et al. Cell 2018). A notable observation is that alloantigen DCs induce alloreactive CD4 T cells eliminate leukemia cells in the setting of allo-HCT (Mochizuki et al. Blood 2016). Intratumoral injection of alloantigen-activated CD4 T cells also reinvigorates host endogenous T cells immunity to eliminate pre-established melanoma and produces an abscopal effect on inducing tumor remission (Mochizuki et al. JECCR 2021, in pressing). Tumor resistance mechanisms can be potentially abrogated upon activation of endogenous immune cells including DCs, macrophages and T cells. Using T cells engineered with CARs and preclinical models, Dr. Zhang and colleagues have established a unique platform to identify epigenetic regulators that enable tumor cells to shape T cell immune phenotype and anti-tumor immunity, and to discover the molecular pathways that mediate epigenetic modulators’ effects (such as EZH2-, DOT1L-, CDK9-inhibitors) on sensitizing tumor immunotherapy.